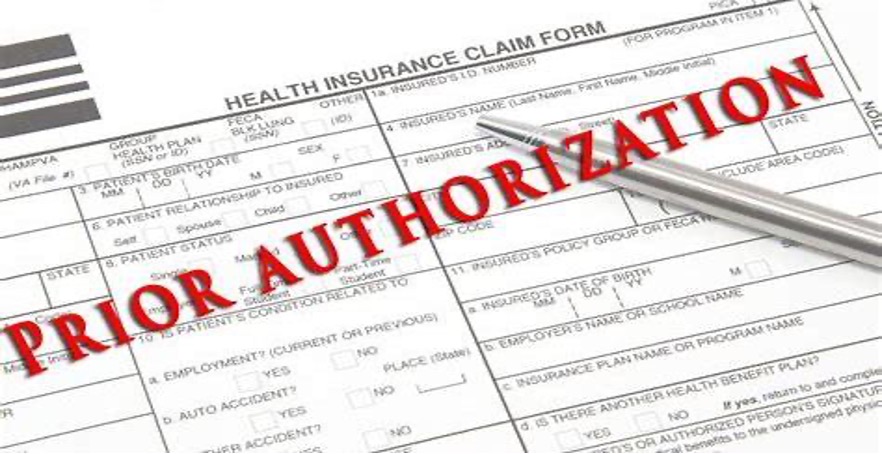
Prior Authorizations are becoming a bigger burden- Now what?

For physicians like Terrence Regan, MD, a Urologist in Florida, prior authorizations are limiting access to important treatments for patients and are draining physician offices of resources and time. According to the American Medical Association, 92% of care delays can be traced back to prior authorization requirements and 1 in 4 patients in 2021 will have been unable to fill their prescription due to a prior authorization.
What you can do?
The Prior Authorization Certified Specialist Program (PACS) has become the #1 training program for allied healthcare providers, pharmacists, and field reimbursement managers. The program is self-paced, online and easy to use. It is currently being used to train field reimbursement specialists and patient access managers across a variety of top 20 pharmaceutical companies.
Request a Quote and learn more about how you can get certified or certify your team/staff.